Treating Chronic Pain
In Australia, many doctors who are specialist pain medicine physicians, such as Dr Simon Tame, are also qualified anaesthetists who have had many years of managing pain.
“My primary specialty is anaesthesia, which is very precise but a little impersonal. The interaction with patients is very fleeting. Pain medicine is very much the opposite. Pain medicine attracted me because it involves complex clinical challenges, and the opportunity to have a longer-term role in patient care. In pain medicine, we don’t have all the answers, and often have to tailor a variety of strategies to help our patients cope better with ongoing pain.
“We use a multidisciplinary team-based approach. Our allied health professionals help patients develop a broader range of strategies for living with pain. Sometimes medications have a limited role, but are generally only useful for short periods of time. For some patients, interventional pain procedures can be very helpful.”
Such is the case for Narelle Newton, who is a patient of Dr Tame’s. In 1998, Narelle had a chair fall out from under her, and as she tumbled to the ground, she struck her head on some shelving. This resulted in muscle injury, as well as damage to her C2 and C3 vertebrae, which caused severe headaches, that for many years were treated with different types of pain medication, sometimes requiring up to eight Panadeine Forte per day.
Over several years Narelle trialled a variety of mild medications, local injections and physical therapy. Whilst there was some improvement for periods of time, this was never sustained, and the impact on her quality of life was severe.
“As the years went by, I starting basing my decision-making around the way the pain affected my life. I would either totally avoid social situations, or if I did go out, I would make sure I had medications with me, knowing I might need to leave if the effect of my headaches became too crippling”.
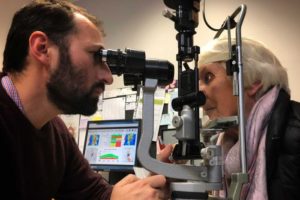
She was then referred to Dr Tame, who raised the idea of using sub-occipital stimulation therapy. This new treatment involves placement of a high-tech device – similar to a pacemaker or cochlear implant – under the skin in the pain area. Whilst the device is only suitable for certain conditions, he thought Narelle might be able to benefit.
The treatment requires significant commitment, and Narelle had to undertake a thorough education session with nurses at Dr Tame’s practice to learn about the treatment process, as well as how to operate the device. She then “trialled” the device for 10 days, which involved a minor procedure and temporary placement of the device, with electronic leads placed underneath her skin in the area immediately under the affected part of her skull. Passing an electrical current through these leads results in a pleasant “buzzing” sensation in the pain area, interfering with the sensation of pain.
The trial was a success – the electrical stimulation significantly improved Narelle’s pain, and she proceeded with a permanent implant, which was inserted through small surgical incisions.
Narelle reports great improvement in symptoms, and is likely to benefit from the device for many years. “I take about three-quarters less medication than I used to, and feel that I am once more in control of my life. I now have the freedom I knew prior to the accident, and am experiencing joy and happiness in my life again. I would encourage anyone suffering the effects of chronic pain to seek the help of a professional to discuss treatment options, rather than relying on medication alone”.
Dr Tame says patients like Narelle are the reason he decided to pursue interventional pain as a specialty.
“Pain medicine is a complex and diverse field, with enormous challenges which I find very stimulating and fulfilling. For Narelle, evolving technology eventually provided her with a treatment that made a huge difference to her life. For many others, a solution has not yet been found – existing treatments are often expensive, and there are few specialists and resources. My hope is that the area of pain medicine becomes a focus for healthcare funding, research and development in the future, and more options become available, so that those suffering from chronic pain are finally able to access treatments that will allow them to live life to the fullest.”